Kenya plans to introduce Lenacapavir, a long‑acting injectable for HIV prevention, beginning in January 2026 a step expected to strengthen adherence, reduce stigma, and extend protection for people at heightened risk of infection. National preparations are under way following approval by the Ministry of Health’s National AIDS and STI Control Programme (NASCOP), positioning the country among the earliest adopters of the twice‑yearly product.
Lenacapavir is given as a subcutaneous injection in the abdominal area twice a year and has shown high protective efficacy reported in studies at up to 99% when used correctly. NASCOP chief executive Dr Andrew Mulwa says the injectable is easier to administer and track than daily pills. The long dosing interval is a major advantage over oral pre‑exposure prophylaxis (PrEP), which many users find hard to maintain because of pill fatigue, stigma, travel demands, or supply gaps in overstretched clinics.
Community experience highlights the stakes. Esther Shiyayo, who has lived with HIV for nearly three decades in a discordant marriage, says her husband’s daily PrEP routine is exhausting; a six‑monthly injection could ease that burden and cut clinic visits. Others in similar situations see the new approach bringing welcome simplicity and privacy.
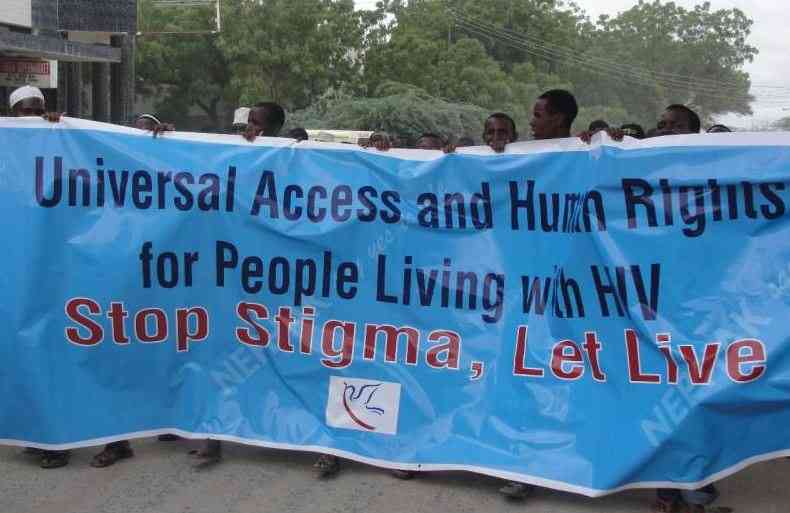
Key populations such as sex workers face even sharper barriers. Everly Nabwire, who leads the NKOKOIJU initiative in Mombasa, reports missed pills after night shifts, stigma when clients see medication, and periodic PrEP stock‑outs. Some members confuse PrEP with antiretroviral treatment. In Nakuru, Smart Ladies chair Daisy Achieng voices similar concerns across a network of more than 17,000 sex workers, arguing that an injectable option would improve adherence and reduce daily stress.
Financing is the central uncertainty. Early access doses are expected through the Global Fund and partners as pricing talks continue with the manufacturer. Nelson Otwoma of NEPHAK says advocates are pushing for costs below high‑income market levels so enrolment can be free in the public system; private purchase could reach $60 per injection. Draft government scenarios suggest programme delivery might land in the $10–$33 per‑person‑per‑year range, depending on region and target group.
Guidelines being finalised will prioritise sexually active individuals at substantial risk. Virologist Prof Omu Anzala notes that Lenacapavir is not a vaccine but an antiviral that blocks the virus like treatment antiretrovirals; reported side effects appear limited. Health officials are building monitoring systems to track uptake, adherence, breakthrough infections, and equity through 2026 and beyond. Strong community feedback loops will be essential.