Uganda is facing an alarming rise in pediatric HIV infections, posing a significant threat to the country’s progress in combating the epidemic. Recent data shows that over 70,000 children aged between zero and fourteen are living with HIV. Additionally, about 1.5 million people across the country are living with the virus, underscoring the urgency of the situation.
One of the most concerning statistics is the annual death toll: more than 3,100 children die from AIDS-related illnesses each year. These deaths point to a silent emergency that could escalate without immediate intervention. Health experts identify mother-to-child transmission as a major contributor to new infections among children. This typically occurs during pregnancy, childbirth, or breastfeeding, especially when mothers lack consistent access to preventive care and treatment.
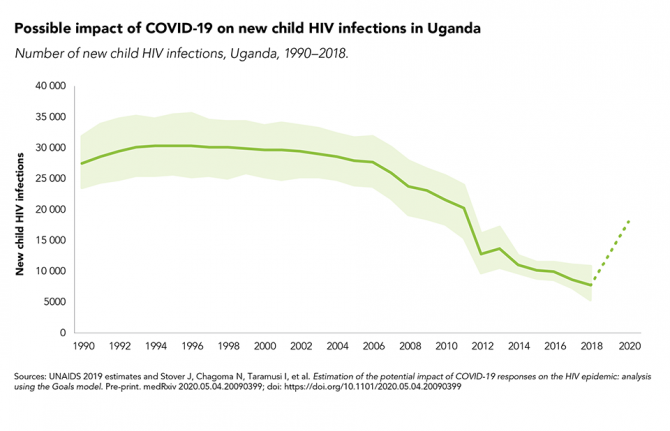
Experts warn that the recent decline in global funding threatens Uganda’s ability to sustain critical HIV programs. Reduced financial support risks reversing progress in early infant diagnosis, treatment adherence, and prevention strategies. Consistent testing and treatment for mothers and children are essential to breaking the cycle of transmission, but without adequate funding, these services remain vulnerable.
Stakeholders are now urging a stronger domestic response to reduce reliance on external donors. Developing a sustainability plan that prioritizes local investment in prevention, treatment, and community health initiatives is seen as a critical step forward. This approach aims to build resilience within Uganda’s health system, ensuring that lifesaving interventions are not jeopardized by fluctuating international aid.
Advocates stress that prioritizing maternal and child health is fundamental to ending the epidemic. Investments in comprehensive care for pregnant women and nursing mothers, coupled with access to antiretroviral therapy, can drastically lower transmission rates and improve survival outcomes for children.
However, time is of the essence. Without renewed funding and strengthened partnerships between the government, civil society, and the private sector, Uganda risks losing even more children to a preventable and manageable disease. Addressing this crisis will require coordinated action, increased domestic financing, and a commitment to ensuring no child is left behind in the fight against HIV.
The path to achieving global HIV targets hinges on protecting the most vulnerable populations, particularly children. Uganda’s future success in controlling the epidemic will depend on bold investments and sustainable strategies that prioritize prevention and care at every level of society.